 Sepsis is a topic that has appeared in the news a lot recently, and the Care Quality Commission (CQC) has recognised the severity of the disease and its effects on our population. The CQC is currently raising awareness in healthcare settings so that healthcare professionals know what signs and symptoms to look out for and act upon.
Sepsis is a topic that has appeared in the news a lot recently, and the Care Quality Commission (CQC) has recognised the severity of the disease and its effects on our population. The CQC is currently raising awareness in healthcare settings so that healthcare professionals know what signs and symptoms to look out for and act upon.
Sepsis can be fatal, but it does not always present with the most obvious symptoms. This means that a diagnosis of sepsis can easily be missed, but it’s crucial that it’s caught as early as possible to improve the patient’s chance of survival. Symptoms can also differ between children and adults, so having a good understanding of the range of symptoms is crucial. The whole dental team should already have received training on sepsis, or training should be scheduled in. If you haven’t received training already, here are some key points about sepsis and what to look out for.
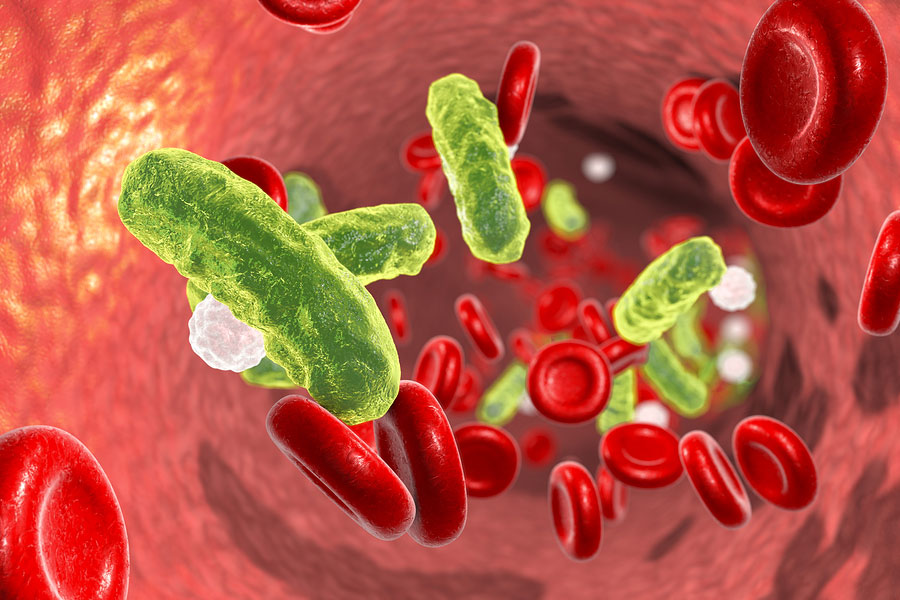
Firstly, what is sepsis?
Sepsis is often referred to as either blood poisoning or septicaemia. It’s when the body’s immune system responds abnormally to an infection instead of fighting any germs (bacteria, viruses, fungi) to prevent infection. The body’s responses go into overdrive, and instead of protecting the organs it starts to attack them, which can lead to tissue damage or multiple organ failure. In some cases, the reaction can be severe enough to lead to death. The infection can start anywhere in the body, and it can either stay localised or can affect the body as a whole.
Sepsis is not contagious; this means that it can not be passed from person to person. However, it can happen as a result of any injury or infection from the following:
- a chest infection causing pneumonia;
- a urine infection;
- a leg ulcer or cellulitis;
- a problem in the abdomen, such as a burst ulcer or a hole in the bowel;
- an infected cut or bite;
- a wound from trauma or surgery.
Sepsis can be caused by a huge variety of different germs, such as E. coli, MRSA, C. diff or streptococcus. Most cases are caused by common bacteria, which normally don’t make us ill.
Who does sepsis affect?
According to The UK Sepsis Trust, there are approximately 123,000 diagnosed cases of sepsis in the UK each year. Sepsis claims an estimated 44,000 lives each year – that’s five people every hour in the UK.
Sepsis can affect anyone, from the very young to the elderly, but there are more cases in adults than in children. People that are at higher risk are those:
- who are pregnant, who have given birth or who have had an abortion;
- who are undergoing chemotherapy for cancer;
- who have had an organ transplant and are on anti-rejection drugs;
- who have had an operation or who have wounds or injuries as a result of an accident;
- who are malnourished (haven’t had enough food);
- who are already in hospital with a serious illness;
- who are immunocompromised and who have health issues such as diabetes.
It’s important to note that only 30% of sepsis cases occur after an operation; 70% of the time, cases occur within the community.
Signs and symptoms
You need to remember the word ‘sepsis’ and remember the key signs to look out for. These have been adapted from: https://www.sepsis.org/faq/
- S-shiver, fever or very cold
- E - Extreme pain or general discomfort
- P- Pale or discoloured skin
- S- Sleepy, difficult to rouse, confused
- I – ‘I feel like I might die’
- S- Short of breath
The key signs of sepsis in babies may include a include a combination of the following:
- no interest in feeding;
- repeated vomiting;
- no consumption of any fluids for more than 8 hours (whilst they are awake);
- no wet nappies for 12 hours;
- a sunken appearance to the eyes;
- floppiness and unresponsiveness.
The key signs of sepsis in children may include:
- rapid breathing or breathing that pauses;
- skin that is cold to the touch;
- a rash that doesn’t blanch;
- lethargy or being hard to wake up;
- mottled, bluish or pale skin;
- fits or convulsions.
Unfortunately, sepsis can often be misdiagnosed as flu, gastroenteritis or a chest infection. Such misdiagnosis and subsequent failure to treat the sepsis can result in septic shock. Signs and symptoms of a person developing septic shock may include:
- feeling dizzy or faint;
- changes to mental state – they may become confused or disorientated;
- diarrhoea;
- slurred speech;
- vomiting or feeling sick;
- severe muscle pain;
- no urination for 18 hours;
- breathlessness;
- loss of consciousness;
- mottled skin or feeling cold, clammy and pale.
If you or your colleagues are at all concerned, it’s important that the patient goes straight to the hospital to get checked or that you ring 111 to get further help and support.
Approximately 50% of patients who are diagnosed with sepsis and are treated do recover completely – but unfortunately, the other half have some lasting effects. These can include:
- post-sepsis syndrome;
- damaged organs, such as reduced kidney function;
- insomnia and fatigue;
- poor mobility or muscle weakness or joint/muscle pain;
- lowered self-esteem;
- nightmares;
- hallucinations;
- panic attacks;
- changes in vision;
- changes in taste perception;
- poor appetite;
- excessive sweating or feeling cold;
- poor concentration;
- short-term memory loss or lack of concentration
Patients should continue to receive support and help for these effect from other health care professionals.
How sepsis affects the dental practice
Finally, the development of sepsis following dental procedures is rare. However, patients who have the following treatments carried out are at a higher risk:
- dental extractions;
- extractions of partially erupted wisdom teeth;
- root canal treatment;
In addition, a patient who presents with an abscess or a pulp infection is at higher risk.
As there is a lot of information to take in surrounding sepsis, it is important that all practices have a procedure in place. (This may be a model procedure which has been downloaded from an appropriate source.) All team members must be familiar with all the warning signs and good teamwork must be ensured so that the team can react quickly if needed.
It’s important to know that when the CQC visits your practice, staff members will be asked what your protocol is and how your practice is managing and referring patients. They will also be asked what aftercare you are giving to patients, so it’s important that in-house training is carried out.
For more information and help with sepsis, please visit the following websites:
https://sepsistrust.org/
https://www.cqc.org.uk/guidance-providers/dentists/dental-mythbuster-25-sepsis
https://www.nhs.uk/conditions/sepsis/
https://www.sepsis.org/faq/
Written by Emma Leather RDN, PTLLS, ACWE, IQA.